Autologous Chondrocyte Implantation (ACI)
Definition of articular cartilage:
The coating on bones in joints that allows them to glide. Cartilage on cartilage is much more slippery than ice on ice. This is very specialized tissue that allows joints to rub without pain or friction. It is usually 4 to 5 mm thick in the knee. It is analogous to the Teflon coating on a pan.
Articular cartilage defects:
These can occur as a result of trauma, overuse, degeneration or arthritis. They cause pain and swelling. Bone is exposed under the cartilage.
Articular cartilage biopsy:
In this procedure, a tiny sample of articular cartilage is taken from a non-weight bearing section on the knee during an arthroscopic surgical procedure. This is the first step in the ACI procedure. The biopsy is flown to the Genzyme Biosurgery Lab in Cambridge, Massachusetts, where the cartilage cells, or chondrocytes, are isolated and frozen.
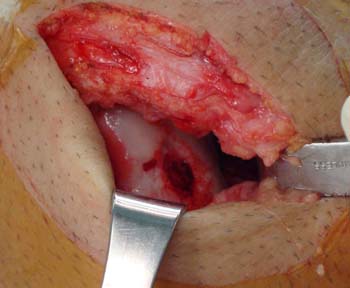 Surgical procedure:
Surgical procedure:
The cartilage cells are grown and then flown back to the Chicago area hospital where they are to be implanted. An incision is made in the knee and the synthetic patch is sewn over the articular cartilage defect. The cartilage cells are implanted under the patch into the defect and are sealed in using a biologic fibrin glue. The patient stays overnight in the hospital and goes home the next day.
Anesthesia:
A general anesthetic (putting the patient to sleep) is usually performed. Alternatively the patient may have an injection into the lower back for spinal or epidural anesthesia. The lower back injections put only the legs to sleep.
Rehabilitation:
The patient stays touch-down (20-30%) weight bearing using two crutches for six weeks, progressing to partial weight bearing for the subsequent six weeks. Depending on the nature of the job, most people return to work during this time. Patients use a continuous passive motion (CPM) machine for six to eight hours per night during the first month or so to help nourish the cartilage cells. This machine is generally used in the evening or during sleep. Full weight bearing is allowed 12 weeks post-surgery. Patients are sent to physical therapy to regain motion and strength. Full activities, including sports, are allowed at 9-12 months after surgery.
Success rate:
In properly selected patients, there is an 85-90% success rate for cartilage regeneration in the distal femur. The success rate for cartilage regeneration in the patella or kneecap is slightly lower. Dr. Lars Peterson, the pioneer of this procedure in Sweden, has conducted follow-up studies of his patients for the past 15 years showing excellent results.
Prevention of arthritis:
We believe that the autologous chondrocyte implantation prevents or slows the progression of arthritis in many or most cases. Longer term results are needed to verify this impression.
Requirements for candidates:
The maximum age for a successful implantation is generally 55 years. If the patient is bowlegged (a varus knee) then a high tibial osteotomy must be done to straighten the tibia. If the kneecap is being operated on, a procedure must be done to take pressure off the patella.
Risks and complications:
There is about a one percent risk of infection that may require further surgery. Some patients may become stiff and require a subsequent arthroscopic procedure to trim scar tissue. Other rare complications such as nerve damage and reflex sympathetic dystrophy can also occur. If the graft fails, the original symptoms may recur and more invasive surgery such as knee replacement may be needed.
Federal oversights:
Autologous chondrocyte implantation is FDA approved for properly selected patients.
Insurance:
Virtually all insurance carriers pay for this procedure in patients who need it.